What is Machado-Joseph Disease?
 Machado-Joseph disease (MJD)—also called spinocerebellar ataxia Type 3 (SCA3)—is one of approximately 30 recognized, dominantly inherited forms of ataxia. Ataxia is a general term meaning lack of muscle control or coordination. MJD is characterized by slowly progressive clumsiness in the arms and legs, a staggering lurching gait that can be mistaken for drunkenness, difficulty with speech and swallowing, impaired eye movements sometimes accompanied by double vision or bulging eyes, and lower limb spasticity. Some individuals develop dystonia (sustained muscle contractions that cause twisting of the body and limbs, repetitive movements, and abnormal postures) or symptoms similar to those of Parkinson’s disease. Others may develop fasciculations (twitching) of the face or tongue, neuropathy, or problems with urination and the autonomic nervous system.
Machado-Joseph disease (MJD)—also called spinocerebellar ataxia Type 3 (SCA3)—is one of approximately 30 recognized, dominantly inherited forms of ataxia. Ataxia is a general term meaning lack of muscle control or coordination. MJD is characterized by slowly progressive clumsiness in the arms and legs, a staggering lurching gait that can be mistaken for drunkenness, difficulty with speech and swallowing, impaired eye movements sometimes accompanied by double vision or bulging eyes, and lower limb spasticity. Some individuals develop dystonia (sustained muscle contractions that cause twisting of the body and limbs, repetitive movements, and abnormal postures) or symptoms similar to those of Parkinson’s disease. Others may develop fasciculations (twitching) of the face or tongue, neuropathy, or problems with urination and the autonomic nervous system.
The clinical manifestations of MJD can be highly variable, even among affected persons in the same family. This wide range in symptoms reflects the particular type of mutation that causes MJD: a repeat expansion in the DNA code that varies in size among affected persons. The longer the expansion, typically the more severe the disease. In other words, longer repeat expansions tend to cause disease that begins earlier in life and shows a broader range of neurological symptoms. In most individuals with MJD, symptoms typically begin in the third to fifth decade of life but can start as early as young childhood or as late as 70 years of age.
MJD is a progressive disease, meaning that symptoms worsen with time. Life expectancy ranges from the mid-30s for those with the most severe forms of early onset MJD to a nearly normal life expectancy for those with mild, late onset forms. The cause of death for those who die early from the disease is often aspiration pneumonia.
The name “Machado-Joseph” comes from two families of Portuguese/Azorean descent who were among the first families described with the unique symptoms of the disease in the 1970s. The prevalence of the disease is highest among people of Portuguese/Azorean descent. For example, among immigrants of Portuguese ancestry in New England, the prevalence is around one in 4,000, and the highest prevalence in the world, about one in 140, occurs on the small Azorean island of Flores. Soon after the gene defect was discovered, a hereditary ataxia in European families known as SCA3 was found to be caused by the exact same mutation. Thus, SCA3 and MJD are the same disorder.
What are the different types of Machado-Joseph Disease?
All persons with MJD have the same disease gene mutation: a DNA repeat expansion in the ATXN3 gene. The wide range in symptoms among affected individuals led researchers to separate the disease into distinct types that are broadly distinguished by age of onset and range of symptoms. Type I MJD is characterized by onset between about 10 and 30 years of age, with faster progression and more dystonia and rigidity than ataxia. Type II, the most common type of MJD, generally begins between the ages of about 20 and 50 years, has an intermediate rate of progression, and causes various symptoms, including prominent ataxia, spastic gait, and enhanced reflex responses. Individuals affected by type III MJD have the latest onset of disease (beginning between approximately 40 and 70 years of age) which progresses relatively slowly and is characterized as much by peripheral neuromuscular involvement (muscle twitching, weakness, atrophy, and abnormal sensations such as numbness, tingling, cramps, and pain in the hands and feet) as by ataxia. Most individuals with MJD, but especially those with types I and II, experience one or more problems with vision, including double vision or blurred vision, loss of ability to distinguish color and/or contrast, and inability to control eye movements. Some individuals also experience prominent Parkinson’s disease-like symptoms, such as slowness of movement, rigidity or stiffness of the limbs and trunk, and tremor or trembling in the hands.
What causes Machado-Joseph Disease?
MJD is classified as one of many dominantly inherited ataxias, specifically the spinocerebellar ataxias or SCAs. In the SCAs, of which nearly 30 separate genetic causes have been identified, degeneration of cells in the hindbrain leads to impaired coordination of movement. The hindbrain includes the cerebellum (a large bundle of brain tissue resembling a bun located at the back of the head), the brain stem, and the upper part of the spinal cord. MJD is inherited in an autosomal dominant pattern, meaning that an affected person has a single disease-causing MJD allele (an allele is half of a pair of genes located at the same position on a person’s chromosomes) and a normal MJD allele, and can pass on either allele to the next generation. Any child of an affected parent has a 50 percent chance of inheriting the disease allele. If the child inherits the disease-causing gene, he or she will eventually develop symptoms of the disease. A child who does not inherit the disease allele will not develop the disease and cannot pass it on to the next generation.
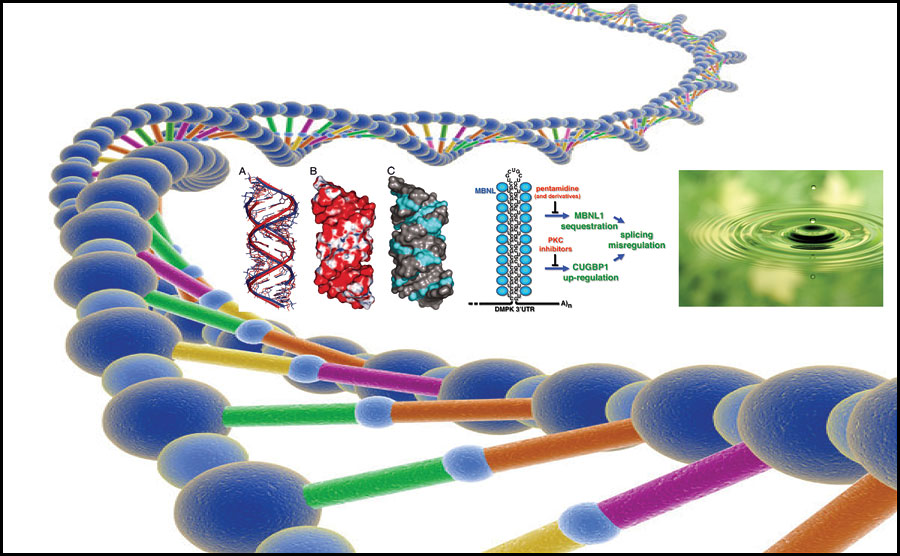
MJD belongs to a class of genetic disorders called expanded repeat diseases. Mutations in expanded repeat diseases are abnormally long repeats of a normal repetition of three letters of the DNA genetic code. In the case of MJD, the code sequence “CAG” is repeated in the ATXN3 gene, which produces the disease protein called ataxin-3. This protein, when mutated, is prone to fold abnormally and accumulate in affected brain cells. The accumulated ataxin-3 protein forms abnormal clumps known as inclusion bodies, which are located in the nucleus of the cell. While the clumps themselves may not be toxic to brain cells, they do reflect a problem in protein folding that likely affects normal properties of the ataxin-3 protein.
One unusual feature of MJD and many other expanded repeat diseases is a phenomenon called anticipation. Anticipation is the remarkable fact that children of affected parents tend to develop symptoms of the disease earlier in life and may experience more severe symptoms. This is due to the tendency for the expanded repeat mutation to further expand when being passed to the next generation, especially when passed from the father. Because longer expansions tend to cause earlier and more severe disease, this molecular growth from one generation to the next likewise causes, on average, an earlier age of onset in subsequent generations. Though longer repeats tend to cause earlier onset disease, it is impossible to predict precisely the time and course of the disease for an individual based solely on the repeat length.
On a worldwide basis, MJD or SCA3 appears to be the most prevalent autosomal dominant inherited form of ataxia.
How is Machado-Joseph Disease diagnosed?
Physicians diagnose MJD by recognizing the symptoms of the disease and by taking a family history. They ask detailed questions about family members who show (or showed) symptoms of the disease, the kinds of symptoms seen in these relatives, the age(s) of disease onset, and the progression and severity of symptoms. A definitive diagnosis of MJD can be made only with a genetic test. The genetic test for MJD (SCA3) is highly accurate. Those individuals who are at risk for MJD (i.e. have an affected parent) but do not have any symptoms can undergo presymptomatic testing to determine whether they carry the disease allele (and thus will later develop the disease). Obtaining presymptomatic testing is a highly personal decision that at-risk individuals should make only after fully considering the potential pros and cons. Many at-risk persons choose not to undergo this test out of concern for job discrimination and difficulty in obtaining or maintaining insurance, among other reasons. For more information on genetic testing and counseling, please consult the organizations listed in the section titled “Where can I get more information?”
How is Machado-Joseph Disease treated?
MJD is incurable, but some symptoms of the disease can be treated. Levodopa therapy (used in treating individuals with Parkinson’s disease) can ease parkinsonian features (stiffness and slowness of movments, often accompanied by a tremor) for many years. Antispasmodic drugs, such as baclofen, can help reduce spasticity. Botulinum toxin can treat severe spasticity and some symptoms of dystonia, but it should be used as a last resort due to possible side effects, such as swallowing problems (dysphagia). Speech problems (dysarthria) and dysphagia can be treated with medication and speech therapy. Wearing prism glasses can reduce blurred or double vision, but eye surgery has only short-term benefits due to the progressive degeneration of eye muscles. Physiotherapy can help individuals cope with disability associated with gait problems, and physical aids, such as walkers and wheelchairs, can assist people with everyday activities. Daytime sleepiness, a common complaint in MJD (as is sleep disturbance in general), can be treated with modafanil and should prompt a formal sleep evaluation. Other problems, such as cramps and urinary dysfunction, can be treated with medications and medical care.
What research is being done?
The National Institute of Neurological Disorders and Stroke (NINDS) supports research on MJD and other related neurodegenerative diseases in an effort to learn how to better treat, prevent, and even cure these diseases. Ongoing research includes efforts to better understand the genetic, molecular, and cellular mechanisms that underlie repeat expansion diseases related to MJD.
Research is now indicating that overlapping mechanisms may be involved in triplet repeat disorders such as MJD, regardless of whether or not the repeat is in a protein-producing or coding region of the gene. Modifications of the mutant protein can impact toxicity, which may explain why some triplet repeat diseases have onset later in life.
Other research areas include the development of novel therapies to treat the symptoms of MJD, efforts to identify diagnostic markers and to improve current diagnostic procedures for the disease, and population studies to identify affected families.
